Findings on imaging
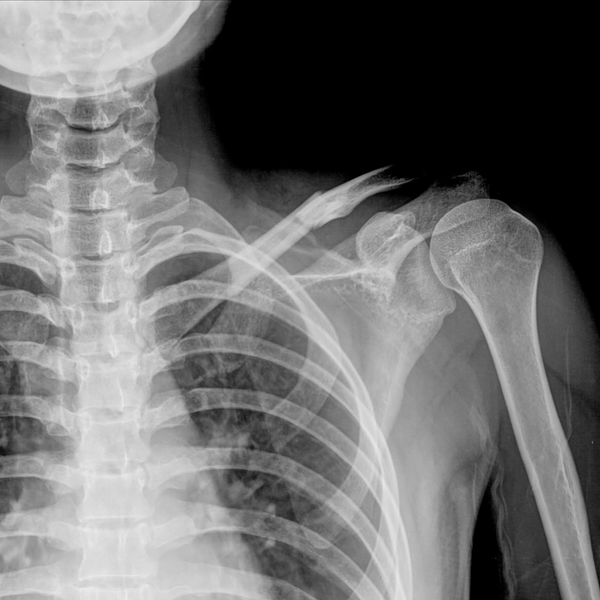
I wanted to take some time to address a common situation I hear in the clinic. It’s related to “findings on imaging,” and what I’m about to say may surprise you. There have been several times where clients come in with imaging such as an MRI, ultrasound, or an X-Ray, which has led to a diagnosis like a disc bulge, degenerative disc disease, a rotator cuff tear, and much more. Does this sound familiar? Maybe this is the situation you currently find yourself in. Having a diagnosis can be scary. Especially if it sounds like something that you will be dealing with for the rest of your life. And you might have thoughts like “there’s nothing that can be done.”
So why do I bring this up? Why do I feel the need to discuss findings on imaging? Well, it’s because there are a lot of misconceptions about what these findings really mean. In physiotherapy, we value evidence just like all other healthcare professions. What does the evidence tell us about findings on imaging? Evidence shows that even people with no pain have positive findings on imaging. For example, one study was done specifically for imaging on patients with no symptoms. Here’s a few highlights from that study.
Disc degeneration showed up in 37% of people aged 20-30, 80% of people aged 50-60, and 93% of people aged 70-80. And this is people with absolutely no symptoms. Disc bulges showed up in 30% of people aged 20-30, 60% of people aged 50-60, and 77% of people aged 70-80! Again, these people have zero symptoms. What does this mean? Imaging does not tell you why you hurt. I’ll explain! If imaging does tell you why you hurt, people who don’t hurt won't have findings on imaging. But that’s not the case at all.
If you like pie, this next part will resonate well with you. Imaging is just one piece of the pie. If you’re in pain, there are a lot of other factors that contribute to your pain experience. Whether that’s how you move, moving too little or too much, other “life” factors such as stress, mood, and much more. I’ll say it again; imaging is just one piece of the pie. And often times, I would argue that it is a small piece of the pie. Yes, imaging has its place and is valuable. Mostly to rule out things like cancer, infection, inflammatory disease, fracture, and severe neurological deficits. But having a positive finding on imaging, other than the conditions just listed, is not guaranteed to be the reason why you’re in pain.
So, what’s my point? Imaging is not the whole picture. Physiotherapists are trained to determine if imaging is required, because imaging is not always necessary according to the evidence. Physiotherapists are trained to identify “red flags” that can be found during an assessment, where a referral for imaging is necessary. They will take a look at the entire picture including your movement, strength, and more to determine the likely contributing factors to your pain, and their goal is to get you back to doing what you love.
At Capture, we try to get you in the doors the day you need care. If you are living in pain, please don’t hesitate to come in for an assessment. We want you to live without pain, let us see what we can do to get you there.
Hope to see you soon!
Curtis Hoyt, Physiotherapist (Provisional)
PS, if you’re interested in taking a peak at the evidence, here’s a few studies that I referred to during this blog post!
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ 2021; 372 :n291. 10.1136/bmj.n291. [PMC free article] [PubMed]
Henschke N, Maher CG, Refshauge KM, et al. . Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum 2009;60:3072-80. 10.1002/art.24853 [PubMed] [CrossRef] [Google Scholar]
Brinjikji W, Luetmer PH, Comstock B, et al. . Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 2015;36:811-6. 10.3174/ajnr.A4173 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
